When you’re sexually active, it’s important to know when to get tested for STDs / STIs. First, tests are only accurate after a certain number of days. Plus, the CDC has guidelines on how often to get tested. Learn when to get tested, possible symptoms, and how soon you can.
✔️ Medically reviewed by Meagan Fleming, RN on April 22, 2019
Do you want to help others know when to test? If this article was useful, please consider sharing or posting it where it can help someone else.
► Herpesyl is the only 100% natural blend that targets the real cause of outbreaks, and weakens and destroys the herpes virus through a 26-plant extract. Click here to get started now.
► Positive Singles is a secure community to meet others with HSV! Dating profiles, blogs and support. Avoid the awkward “talk” and Sign up free!
About Getting Tested for STDs / STIs
If you’re sexually active and at risk, the time to get tested is now. One out of two people will contract an STI by age 25, and half of all Americans will get an STD at some point in their life (1). Plus, many STIs have no symptoms.
That’s why sometimes instead of testing for certain STIs, you can be screened for several at once. You can do that by getting a test called a full panel.
What is Included in an STD Panel?
A typical full-panel STD test includes a urine test for Chlamydia and gonorrhea, and a blood test for HIV, syphilis, and hepatitis B and C. It doesn’t always include all STIs. In fact, practitioners often won’t include a test for herpes unless you already have a sore. (2)
Does a Pap Smear Include an STD test?
No, a pap smear does not include an STD test. A pap smear looks for abnormal cells on the cervix as a screening tool for cervical cancer. (3) Tests for chlamydia, gonorrhea, HIV, syphilis, and hepatitis need to be done with blood and urine samples.
STD Testing by Population:
- Pregnant Women: The CDC recommends that all pregnant women be screened for syphilis, HIV, and Hepatitis B (4). For women with higher risk factors, Chlamydia and gonorrhea tests early on in the pregnancy.
- Sexually active women under 25: Yearly testing for Chlamydia, gonorrhea.
- Everyone 13-65: Test for HIV at least once.
- People who have unsafe sex: Get screened for HIV annually. Also be screened for Chlamydia, gonorrhea, and syphilis.
- Sexually active men who have sex with men: HIV testing every 3-6 months would be beneficial, according to the CDC. (5)
- Baby Boomers (1945-1965): Baby boomers have a high rate of Hepatitis C. In fact, 75% of cases are in this generation. (6)
When to Get Tested for STDs / STIs
In general, everyone under 25 should be tested annually. And everyone over the age of 25 who is at increased risk should also be tested annually.
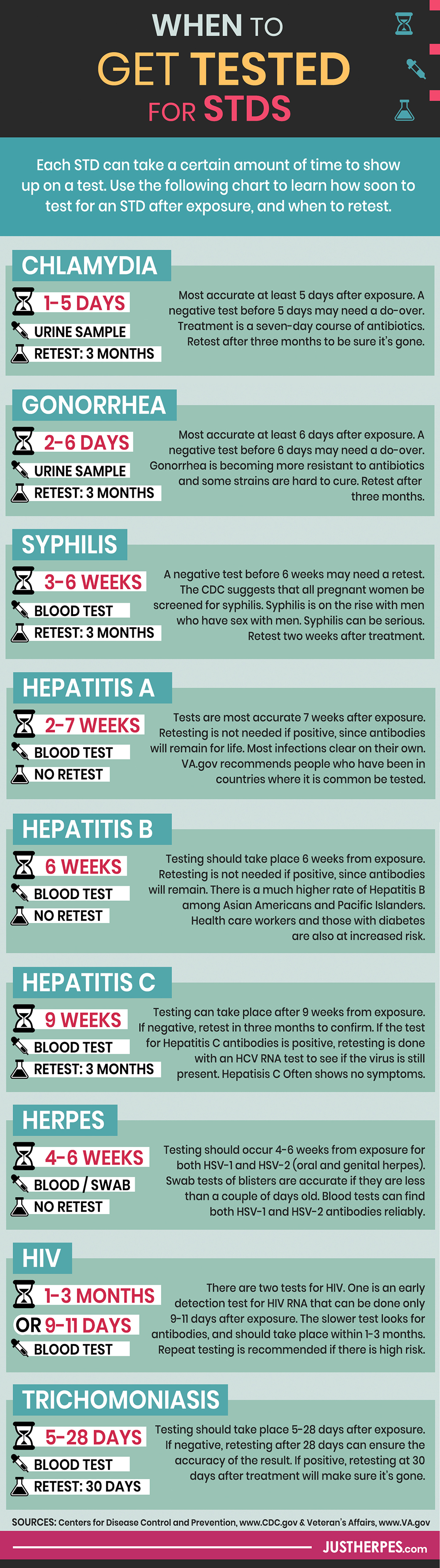
For individual STIs, there are guidelines for testing each one based on the time of its “incubation period”. That means it takes a certain amount of time for each infection to show up on a test. You can see a list as follows.
There are also general recommendations for STD testing for those that are sexually active regardless of exposure risk. These come from sources like the CDC, which provides screening recommendations for healthcare providers.
1. Chlamydia:
- When to Test for Chlamydia: Chlamydia testing can take place within 1-5 days from exposure, but is most accurate after 5.
- Retesting: If negative, retesting needs to occur after 5 days have elapsed. If it comes back positive, you should retest 2-4 weeks later to ensure the Chlamydia trachomatis bacteria is clear from your system.
- How Often: The CDC recommends men and women at increased risk need to be tested every 3-6 months, and that sexually active women under 25 years be screened for Chlamydia annually (7). This disease is also tested during the initial pregnancy screening then again in the third trimester.
- Type of Test: Urine. You can urine test for gonorrhea and Chlamydia at the same time.
- Symptoms of Chlamydia: Often has no symptoms.
- Complications from Chlamydia: Chlamydia increases the risk of reproductive complications like infertility or ectopic pregnancy. It can also lead to pelvic inflammatory disease. If passed to an infant during childbirth, the infant could be at risk for ophthalmia neonatorum (conjunctivitis), or even pneumonia. (8)
- Treatment: Treatment is quick and painless, with a seven-day course of antibiotics. Sex partners should also be treated, as re-infection is common. Re-test after three months to be certain it’s gone. (9) (10)
2. Gonorrhea:
- When to Test for Gonorrhea: Testing can take place within 2-6 days from exposure. Sexually active women under 25 years of age are recommended to be tested annually. The CDC recommends men and women at increased risk need to be tested every 3-6 months.
- Retesting: If negative, retesting needs to occur after 6 days have elapsed. When positive, after treatment retesting should occur 3 months later to ensure it’s gone.
- Type of Test: Urine. In some cases, a swab may be used. You can urine test for gonorrhea and Chlamydia at the same time.
- Symptoms of Gonorrhea: Gonorrhea often shows no symptoms. Symptoms include painful or burning sensation when urination, discharge (men and women), or spotting/bleeding between menstrual periods. When affecting the rectum, symptoms can include discharge, itching, pain, and bleeding.
- Complications from Gonorrhea: Successful treatment doesn’t reverse permanent damage caused by the infection. Left untreated, it can cause Pelvic Inflammatory Disease in women, ectopic pregnancy, infertility, and pelvic pain. Gonorrhea can be passed to a baby during childbirth.
- Treatment: Gonorrhea has been curable for decades, but reports continue to emerge of antibiotic-resistant gonorrhea, which will make curing it more difficult. (11) (12)
3. Syphilis:
- When to Test for Syphilis: Testing can take place within 3-6 weeks from exposure.
- Retesting: If negative, retesting needs to occur after 6 weeks have elapsed. When positive, after treatment retesting should occur 2 weeks later to ensure clearance of the bacteria Treponema pallidum from your system.
- How Often: This disease is also tested during the initial pregnancy screening then again in the 3rd trimester. The CDC recommends men and women at increased risk be tested every 3-6 months. (33)
- Type of Test: Blood test. Occasionally, by swab of a sore.
- Symptoms of: Can have no symptoms. It can start with sores that are usually round, painless, and firm. As it progresses, symptoms include rashes, swollen lymph nodes, and fever. (13)
- Risk factors: Treatment and prevention once made syphilis rare in the United States, but is now on the rise with men who have sex with men.
- Complications from Syphilis: Tertiary syphilis has severe complications like heart, brain, and other organ problems. Neurosyphilis can occur at any time through the above stages. It affects the brain and nervous system or eyes, affecting muscle coordination, numbness, and cognition (14).
- Treatment: If caught early, syphilis can be cured with a single injection of Benzathine penicillin G. Late syphilis can be treated with similar injections, weekly for three weeks. (15).
4. Hepatitis A:
- When to Test for Hepatitis A: Testing can take place within 2-7 weeks from exposure. If negative, retesting needs to occur after 7 weeks have elapsed.
- Retesting: Retesting is not necessary if positive, as your body will continue to produce antibodies and test positive for life. (16)
- Type of Test: Blood test. IgM antibody.
- Risk Factors: Living or traveling in countries where Hepatitis A is common, or being in close contact with someone who does. Men who have sex with men, having a sex partner you know has it, drug use, or clotting disorders like hemophilia.
- Symptoms of: Usually makes people feel sick with yellowing of skin and eyes, abdominal pain, loss of appetite, dark urine, nausea, diarrhea, low-grade fever, and feelings tired. Some people don’t feel ill or have symptoms at all (17).
- Complications: Can result in hospitalization.
- Treatment: Hepatitis A infections will typically clear on their own in healthy individuals without treatment other than rest and getting lots of fluids. (18)
5. Hepatitis B:
- When to Test for Hepatitis B: Testing should take place 6 weeks from exposure.
- Retesting: Retesting is not necessary if positive, as your body will continue to produce antibodies and test positive for life. This disease is also tested during the initial pregnancy screening, with retesting at delivery in high-risk mothers.
- Type of Test: Hepatitis blood panel.
- Symptoms of: The CDC says while many do not have symptoms, 70% of people with an acute hepatitis B infection will. Symptoms might include fever, fatigue, loss of appetite, stools that are clay-colored, dark urine, yellowing skin or eyes, vomiting, nausea, or abdominal pain.
- Risk Factors: Some populations are at greater risk.
- Asian Americans and Pacific Islanders have a far higher rate of Chronic Hepatitis B. At only 5% of the United States population, API account for more than half of the total cases of chronic hepatitis B in the country. Thus, the CDC has strong recommendations for screening in this population. (19)
- Health care workers and patients can be at risk of hepatitis B from errors in protocol. (20)
- People with diabetes type 1 or 2 have a higher incidence of hepatitis B than others, particularly so if sharing blood monitoring or insulin devices. (21)
- Complications: 15-25% of those with untreated hepatitis B develop cirrhosis, liver damage, or in some cases, liver cancer. (22)
6. Hepatitis C:
- When to Test for Hepatitis C: Testing can take place 9 weeks from exposure. Retesting needs to occur if negative after 3 months to confirm initial results.
- Risk Factors: Baby boomers have a high rate of Hepatitis C. In fact, 75% of cases are in this generation (23). Those with symptoms associated with liver disease may also need a test for Hepatitis.
- Type of Test: Hepatitis blood panel. Antibody test to test for past exposure. If positive, a second test (HCV RNA) will be done to check if you still have the virus. That’s because one out of five people will clear the virus without treatment. For others, it can become chronic.
- Symptoms of Hepatitis C: Many people with chronic Hepatitis C will have no symptoms for years. Symptoms of acute infection can include fever, joint pain, abdominal pain, nausea, dark urine, and jaundice.
- Complications from Hepatitis C: Chronic infections can lead to GI bleeding, abdominal swelling, and cognitive changes. Chronic infections can lead to cirrhosis of the liver. (24)
7. Herpes (HSV-1 and HSV-2):
- When to Test for Herpes: Testing should take place after 4-6 weeks from exposure for the blood test. However, currently the CDC does not recommend this test unless there are symptoms present or similar cause for concern.
- Retesting: Repeat testing is positive is unnecessary, as those with herpes will continue to test positive for the antibodies for life. However, you can retest if you want to make sure you did not receive a misdiagnosis like a false negative or a false positive.
- Type of Test: Blood test, or swab. If you have a sore, doctors can swab it, but it must be done within two days of the sore appearing to be reliable.
- Symptoms of Herpes: Cold sores on the mouth, or sores on the genitals, buttocks, or thigh.
- Risks from Herpes: It is possible to have children if you have herpes, however herpes can cause complications if passed from mother to child during childbirth. Therefore, a doctor may recommend a c-section.
- Treatment: There is currently no cure for herpes. Herpes outbreaks can be stopped or reduced with antiviral medications like acyclovir and valacyclovir (Valtrex). (25)
8. HIV:
- When to Test for HIV: Testing should take place within 1-3 months from exposure when using the HIV antibody test method. There is also an early detection HIV RNA method where the minimum testing period is reduced to 9-11 days, which is obviously a good option if you have reason to believe you have been exposed.
- Retesting: Repeat testing at 3 months and 6 months if previous tests are negative is recommended if there was significant risk. This disease is also tested during the initial pregnancy screening, with retesting at delivery in high-risk mothers.
- Type of Test: Blood.
- Symptoms of: Some people don’t have symptoms that clue them in to contracting HIV. Others, though, can have flu-like symptoms 2-4 weeks from exposure. (26)
- Risks from: AIDS; highly contagious.
- Treatment: There is no cure for HIV, but antiretroviral therapy (ART) is available and should be started immediately. A treatment called PEP can be given in cases where contact was just made with the virus to prevent HIV (27). For regular prevention, another treatment called PrEP can reduce the risk of getting HIV from sex by 90% (28).
9. HPV / Genital Warts:
- Testing: There isn’t a routine screening for HPV, even though it’s the most common STI and most sexually active people will get it. There are tests recommended for women 30 and older for high-risk strains of HPV. They are performed using cell samples from the cervix that look for changes of those cells. Typically, this test will only be done after a Pap test shows abnormal cells, to find out if they are caused by risky / cancer-causing strain of HPV (17). An HPV test may be done along with a Pap test, or by itself. There is also a certain type of Pap test that can be used to check for HPV as well, called a liquid-based Pap (18). The test is not done on men.
- Symptoms: Many types of HPV cause no symptoms, while others cause warts or cancers. Genital warts can have many appearances. Some are flat and white, some are raised, and some aren’t visible at all. There may be other signs like pain, itching or bleeding anytime from 3 weeks to years after contracting HPV. Due to the limited testing, usually people find out they have it when they get either genital warts or cervical cancer.
- Vaccines: Vaccines for HPV include Cervarix, Gardasil, and Gardasil 9.
- Treatment: There is no cure for HPV. (29)
10. Trichomoniasis:
- When to Test for Trichomoniasis: Testing should take place 5-28 days after exposure. If negative, retesting needs to occur after 28 days. When positive, after the treatment course, there needs to be a retest at 30 days to ensure clearance of the causative organism.
- Type of Test: Pelvic exam for women; urethral exam or urine test for men.
- Symptoms of: Most people have no symptoms. When there are symptoms, they can include burning or discomfort during or after urination, itching, irritation, and discharge.
- Risks from: Can increase the risk on getting other STDs, and can lead to early labor in pregnant women and low birth weight.
- Treatment: Trichomoniasis can be cured with an oral antibiotic. (30)
Understanding STD Test Results
Negative test results will read as either negative or non-reactive.
All laboratory testing has a small chance of failure, causing “false positive” or “false negative” results. If you doubt your test results, discuss this possibility with your physician. There may be a need to repeat these tests.
Some Special Considerations
- Sexual assault requires immediate baseline testing after the incident. (31)
- Those that are at increased risk for STDs are typically tested more frequently as well. Some of these risk factors include multiple sex partners, men who have sex with men, partners with known STD infections and work in the sex industry.
- If you believe you have been exposed to HIV, speak to a doctor immediately. Time is of the essence, as sometimes early antiretroviral therapy drug intervention can prevent it.
When can STDs be transmitted?
Sexual contact including vaginal, anal, and oral can potentially transmit an STD. Ejaculation is not necessary for an STD to be transmitted. Usually longer and repeated sexual contact can lead to a high rate of exposure – however any sexual contact, no matter how brief, has the potential to transmit an STD.
Barrier protection such as condoms is useful for decreasing the chance that an STD is transmitted. However, barrier protection can fail from manufacturer defects or damage during intercourse. Additionally, skin infections like herpes can be transmitted even with a condom if the virus affects skin around the covered area.
The bottom line is that if you are having any sexual contact with someone that has an STD, there is a chance that you could get it. Remember: a person can have an STD and not display any symptoms. (32)
Where Can I Get Tested for STDs / STIs?
Your general practitioner, OBGYN, or urgent care clinic can all order STI / STD tests for you. You can also try a local or campus clinic or your local Planned Parenthood location.
Depending on your income, you may even be able to get tests for free. Search here for your local Planned Parenthood and call to find out if you qualify for free testing.
If you’re uncomfortable with those options, or don’t want STI tests on your insurance, some states allow you to order tests at home.
You can also order a testing kit and test yourself at home. Our affiliate myLAB Box can send you one now. Just pick the type of test you want. It won’t have to show up on your records or insurance.
Same-day testing today: You can also use this site to order tests online and then stop by a lab near you for same-day testing.
Final Words
With safe sex, the odds are usually in your favor. Knowing how soon to get tested after exposure, and when to get tested for STDs, also makes a difference. Overall practicing safe sex and alerting your physician when you believe you are at risk for STD exposure is ideal.

► Herpesyl is the only 100% natural blend that targets the real cause of outbreaks, and weakens and destroys the herpes virus through a 26-plant extract. Click here to get started now.