Herpes viral shedding refers to a stage of herpes when the virus becomes active on the skin surface and is contagious. Sometimes, it is asymptomatic viral shedding. Viral shedding with no outward signs leads to the possibility of silent transmission of herpes to unknowing partners. So how often does viral shedding happen, and how can you be both aware and safe?
✔️ Medically reviewed on May 7, 2019
What is Viral Shedding?
Herpes viral shedding refers to any time the herpes virus becomes active and contagious. The virus hibernates in nerve cells until it decides it’s time to surface to the skin and potentially spread to others through skin-to-skin contact. It’s easiest to know herpes shedding is happening when there is a visible outbreak, and thus to avoid sex or contact with the area. Visible outbreaks appear as red, raised, oozing, or crusted nodules.
But other times, viral shedding is difficult to pinpoint. When the virus is active and contagious, but there are no symptoms, it’s known as asymptomatic shedding or subclinical shedding. With no outward signs, it’s easy for the virus to spread to unknowing partners — especially when about 85% of people with herpes don’t know they have it (1). Asymptomatic herpes is likely one major reason the virus is under-diagnosed.
The bottom line is that it’s clear that avoiding sex during visible outbreaks isn’t bulletproof.
Rates of Herpes Viral Shedding
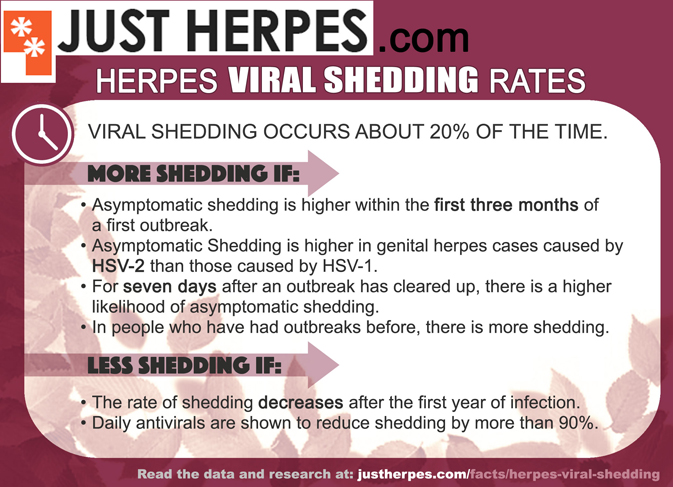
Asymptomatic viral shedding occurs about 20% of the time in people with HSV-2 genital herpes, according to one study. However, the study and others like it uncovered factors that influence this rate. One particular study of women as published in the Annals of Internal Medicine made some interesting findings about shedding frequency (2).
- Asymptomatic shedding is higher during the first three months of contracting the virus, suggests the Annals of Internal Medicine study. “Asymptomatic cervical shedding was 3 times more frequent during the first three months after resolution of primary type 2 disease than during later time periods,” it says.
- Asymptomatic shedding occurs more with genital herpes caused by HSV-2 than genital herpes caused by HSV-1, according to the same study.
- Women previously infected with HSV-1 (usually associated with cold sores) before acquiring HSV-2 may have a lower rate of asymptomatic genital shedding. “Among patients with type 2 infection, previous type 1 antibody was associated with a lower rate of asymptomatic vulvar shedding.” (However, another study suggests no difference.) (3)
- People with cold sores caused by HSV-1 can transmit the virus to the genitals via oral-genital sex.
Studies that test shedding using the Polymerase Chain Reaction method show a higher rate of shedding than studies that test cultures. For example, the study above was based on PCR testing and showed a 20% rate of herpes shedding. Tests that use cultures, on the other hand, suggest that shedding occurs approximately 3% of days (4). However, PCR is more sensitive and therefore we would assume the results of these studies to be more reliable. Nonetheless, there are some pertinent conclusions to be drawn from studies that use culture testing.
- The rate of herpes shedding decreases after the first year of infection, according to studies and papers: “Among 227 women with primary genital HSV-2 infection, the rate of shedding from the cervix or vulva decreased from 3.1% of days during the first year, to 2.3% during the second year and 2.1% during the third year.” (4)
- Persons who have HIV as well as herpes experience more frequent viral shedding (4).
Another 2011 study used a much larger sample size of 498 HSV-2 infected persons, and also said viral shedding occurs about 20% of days (3). However, this study included viral shedding that accompanied outbreaks. The study noted that people who tested positive but never experienced herpes symptoms were shedding 10% of the time (3). The researchers explain that this is because the outbreaks count as times when the virus is shedding. So, according to this paper:
- There was a 20% rate of shedding if a person has outbreaks.
- There was a 10% rate if they never have outbreaks.
Not only is there a difference in shedding rates between people with symptomatic and asymptomatic herpes infections, it also matters how many outbreaks you have per year. “Persons with 8 or greater recurrences per year had a viral shedding rate of 18.9% vs 12.7% among persons reporting 1 to 7 recurrences per year,” say the researchers in the study (3).
How Long Does Herpes Shedding Last?
A 2008 study published in the Journal of Infectious Diseases measured the duration of “reactivations” of HSV in healthy adults. The sample size included 25 people who tested positive for HSV-2, who were checked via swabs four times a day for 60 days. These were the findings (5):
- 24% of the genital herpes reactivations lasted 6 or fewer hours.
- 49% of the herpes shedding periods lasted 12 or fewer hours.
- Only 7% were accompanied by visible lesions.
How to Know if You’re Shedding
Apart from abstaining from sex during an outbreak, when else should you abstain? How do you know if there are no symptoms? It’s hard to do most of the time, and impossible all of the time. A study in the Journal of Antimicrobial Chemotherapy states that asymptomatic patients can be educated about signs of shedding to be more aware of when the virus has become active, but that these silent recurrences can still go under the radar (4). And currently, there is no herpes shedding test kit to help us out.
Nonetheless, there are things to look out for and be aware of.
- Avoid sex for at least a week after any visible outbreaks. A 1995 study in the New England Journal says asymptomatic shedding frequently happens within days of a visible outbreak. “Half the episodes of subclinical shedding of HSV occurred within seven days of a symptomatic recurrence. The risk of subclinical shedding increased with the frequency of symptomatic recurrences.” (6) Even after a herpes outbreak has cleared up, a heightened risk of transmission may remain for another week.
- Be aware of your prodromal symptoms. If you’ve ever had an outbreak, there could have been warning signs, such as tingling, burning, discomfort, or fatigue. If you’ve never had an outbreak, be aware of those signs or of an increase in day-to-day stress, which can be an outbreak trigger. For example, more unusual symptoms of herpes could include nerve pain in the leg. Sometimes asymptomatic carriers of herpes realize they do have symptoms after all once they are educated about them.
- Know typical herpes outbreak triggers and avoid them as often as possible. This is standard protocol for people who want to lessen their outbreaks, but perhaps the same logic could be applied to avoiding asymptomatic shedding as well. The most common triggers of herpes activation are stress, a diet with too much arginine, too much UV light, and irritation to the area of infection. Eat a diet for herpes outbreak prevention, avoid triggers, and manage stress.
90% Drop in Shedding (And 1% Transmission Rate)

Couples in which one partner has herpes and the other doesn’t can vastly reduce their likelihood of transmitting the virus. This can be done with suppressive therapy, condom usage, and avoiding sex during high-risk periods like outbreaks.
Antiviral suppressive therapy means taking a medication like acyclovir or valacyclovir (Valtrex) on a daily basis. Doing so drastically reduces outbreaks and periods of contagiousness. One study found that valacyclovir and acyclovir caused at least a 90% reduction in asymptomatic viral herpes shedding in test subjects (4). (Please note that this quote refers to testing of cultures instead of PCR testing, which is why it doesn’t attest to the 20% rate of shedding in the more sensitive studies.)
Asymptomatic shedding accounted for nearly half of the total viral shedding noted during the trial. In an intent-to-treat analysis, asymptomatic shedding was detected on 6.9% of days for placebo and on 0.3% of days for acyclovir—a 94% reduction. Reduction of asymptomatic shedding was noted at all anatomical sites. When analysed by PCR, the shedding rates for individual women were reduced by a median of 80% (range, 34–91%). Among specimens that contained HSV DNA, treatment with acyclovir reduced the amount of DNA detected by 90%.” (4)
Coupled with condom usage, which reduces the risk by 30%, or up to 50% in some studies, you can bring the risk down more. A study by the makers of Valtrex suggests that you can manage your risk of transmitting herpes to your partner all the way down to 1% or 2% if you use daily antivirals, condoms, and avoid sex during outbreaks.
In an independent, breakthrough study conducted in 2004 by Cory et al., daily suppressive therapy with valacyclovir reduced the frequency of viral shedding in HSV-2 infected individuals and significantly reduced the transmission of genital herpes infection among heterosexual, monogamous partners where one had HSV-2 and the other did not. The rate of transmission of HSV-2 by susceptible partners was reduced by 48% and the occurrence of clinical disease was reduced by 75%. With daily valacyclovir therapy, viral shedding was detected on 2.9% of the days for HSV-2 infected people who received the drug compared with 10.8% of days among those who received placebo.
The above studies enlighten us that not only should you avoid sex during outbreaks, but also at least one week after the outbreak has cleared, and within the first three months of a first-ever herpes outbreak.
Ongoing research is studying possible future treatments that may be able to be used in conjunction with antivirals to lower the risk even further.
Summary
Asymptomatic viral shedding is one of the reasons herpes can be as common as it is and yet under-diagnosed. With the above studies, we learn that people unaware of their status because of having no obvious symptoms are likely to be contagious less of the time. Yet due to this lack of awareness, they may transmit the virus more often.
We also learn that herpes viral shedding periods lessen over time, although herpes shedding continues to occur.
Luckily, with awareness and precaution, it’s possible to manage your transmission risk down so much that it’s possible to carry on a normal sex life without giving your partner herpes.